Today marks the eighth anniversary of The Affordable Care and Patient Protection Act, commonly known as the ACA, which was signed into law March 23, 2010. The law promised to make health care more affordable and accessible for millions of Americans and, eight years later, more Mainers have health insurance than before the law’s passage.
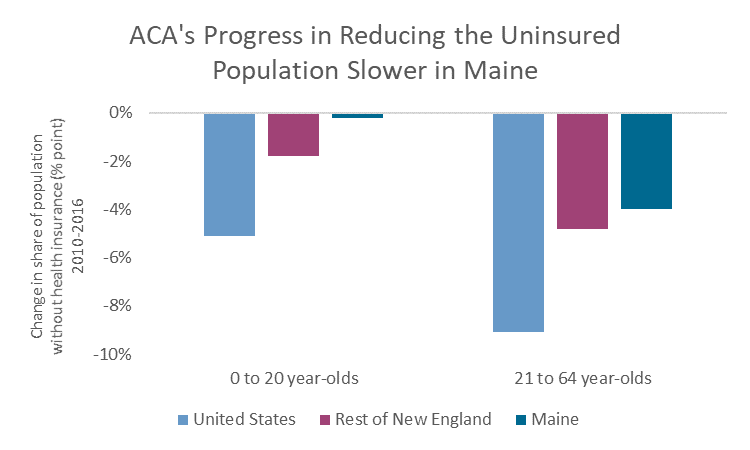
While the ACA was not a panacea to cure all the ailments of the United States’ health care system, the law’s success at increasing coverage is undeniable. However, progress in Maine has come at a slow pace, thanks in part to state-level policy decisions to cut access to Medicaid at a time when other states were expanding health care by increasing eligibility for the program under the auspices of the ACA. No other state has reduced access as dramatically as Maine, and tens of thousands have lost insurance coverage as a result.
The state’s decision to restrict eligibility for Medicaid, rather than expand it as the ACA allowed, limited the success of the landmark federal health care law in Maine. However, Maine voters recent vote to approve Medicaid expansion is poised to make up for years of lost progress.
Insurance coverage grows under ACA
One of the primary goals of the ACA was to improve health insurance coverage for Americans. It did so through a combination of incentives (subsidies, guaranteed minimum provisions) and mandates (for individuals and employers).
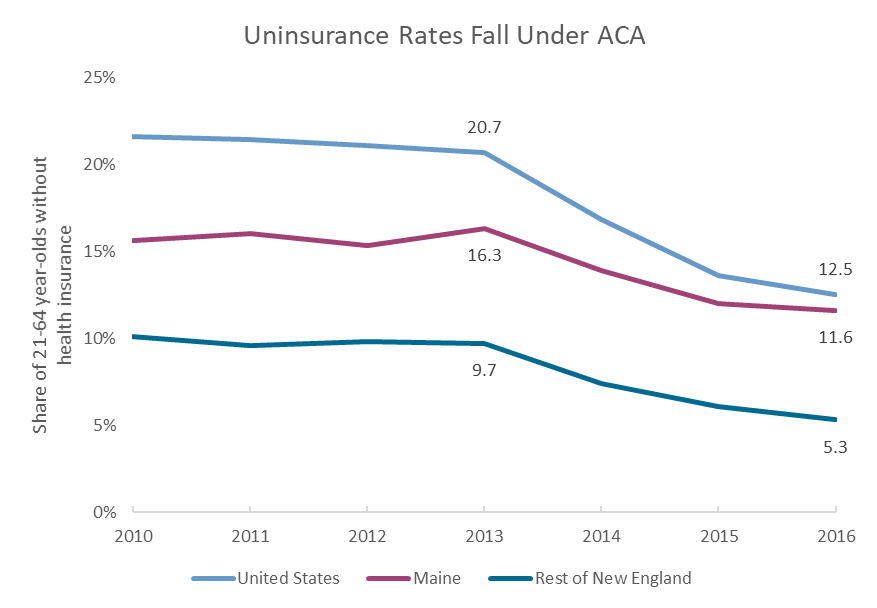
Since 2010, tens of millions of Americans have gained insurance coverage. In Maine, an additional 31,000 adults between the ages of 21 and 64 have insurance today, compared to 2010 coverage rates.[1] Even more Mainers, including those who had coverage before implementation of the ACA, have benefited through expanded benefits and premium subsidies.
More than 70,000 Mainers have signed up for coverage through the federal health insurance marketplace. Many of these Mainers were previously insured but benefitted from provisions of the ACA that reduced out-of-pocket costs when they switched to plans sold on marketplace. Eighty-four percent received some sort of financial assistance in purchasing an insurance plan, with an average of more than $400 toward their monthly premiums.
The hundreds of thousands of Mainers with plans through their employer benefited from consumer protections such as the end to lifetime limits on care, expanded coverage for young people on their parents’ plans, and an expanded list of essential health benefits.
Source: MECEP analysis of US Census Bureau, American Community Survey, 1-year data
While many of the new patient protections took effect immediately when the law was signed, most of the increase in insurance coverage came after 2014, with the implementation of the federal marketplaces and subsidies for individuals to buy health insurance. Many of the minimum requirements for insurance plans (e.g. no disqualification for pre-existing conditions) also took effect in 2014.
Before those key ACA provisions were implemented, the share of nonelderly adults in Maine without insurance had been increasing, even as it declined nationally and regionally.
That trend was driven in large party by Maine Gov. Paul LePage’s changes to Medicaid eligibility, which resulted in 25,000 people losing access to the program in 2013. The governor’s efforts held Maine back from expanding health insurance coverage at the rate of other states. The Medicaid changes, which were aimed at parents and non-disabled adults without dependents, had knock-on effects on children’s health insurance. Research shows that children are eight times more likely to be insured if their parents have insurance. In 2016, the share of children with health insurance in Maine was statistically the same as the share in 2010, with any gains from the ACA wiped out by a surge in uninsured children between 2010 and 2015.
Source: MECEP analysis of US Census Bureau, American Community Survey, 1-year data
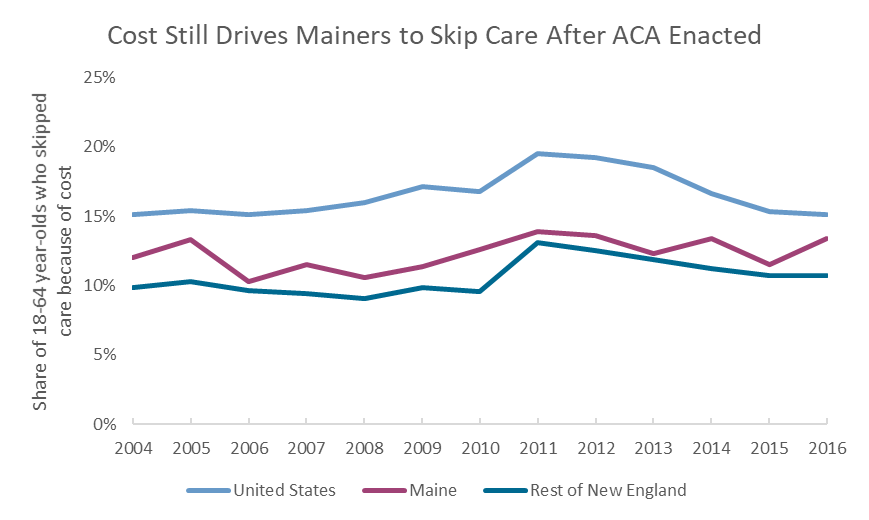
Cost still a barrier to care
Health care, however, is about more than just health insurance. Coverage is only useful if enrollees can afford to avail themselves of the services it provides.
In this, the ACA’s success has been more mixed. In 2011, just after the ACA was signed, nearly one in five Americans had to miss or delay a doctor’s appointment because they couldn’t afford it. By 2016, this share had fallen to one in six.
This progress, however, only brought health care affordability rates back to pre-Recession levels. The same share of Americans skipped care because of cost in 2006. The trend in New England was similar, with the ACA improving affordability, but only to pre-Recession levels.
In Maine, affordable care has remained out of reach for many in the post-ACA era, thanks again to the state’s backward approach to Medicaid. Immediately before the 2008 recession, 10% of Mainers skipped care because of cost. That number rose to 14% by 2011 and remained at 13% in 2016. Again, the decision to strip tens of thousands of Medicaid coverage made health care less affordable, even for those individuals who were able to regain insurance through private plans.
Source: MECEP analysis of US Centers for Disease Control, Behavioral Risk Factors Surveillance Survey
A good start, not a finish
Fully implementing the will of Maine’s voters and enacting Medicaid Expansion will provide health insurance to an additional 70,000 Mainers — a boom in coverage that will help Maine catch up to the rest of the country and our neighbors in terms of access to care. But even with Medicaid expansion, there will still be tens of thousands of Mainers without insurance, and many insured Mainers who still can’t afford care.
The health care picture in the United States, and in Maine, is rosier today than it was eight years ago. However, we have not yet achieved a world of universal coverage and affordability. That means policymakers, at the state and federal level, still have work to do. The ACA provides a solid foundation for the work ahead.
Footnotes
[1] Based on a drop in the uninsured rate from 15.6% to 11.6% of the 21 to 64 year-old population.